CONTACTStaffCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2024 Pride Publishing Inc.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Private Policy and Terms of Use.
Virtually all deaths from cervical cancer are preventable, yet the disease will kill almost 4,000 women in this country this year. Frustrated scientists know who most of them will be: African-American women in the South, Latinas along the Texas-Mexico border, white women in Appalachia and the rural Northeast, and Vietnamese immigrants.
Efforts are under way to reach those women, including a $25 million federal program poised to let communities recruit volunteers--women who speak their patients' language and can engender trust--to encourage Pap testing and shepherd the newly diagnosed through an often baffling medical system.
It's work made more urgent by the discovery that a high incidence of cervical cancer is a red flag for other health disparities: The same localities also have excessive rates of breast and colorectal cancer, strokes, and infant mortality.
The new report, from the National Cancer Institute, will "hopefully ring a bell for policy makers" in those communities, says Harold P. Freeman, a cancer specialist who works in Harlem, N.Y., and directs NCI's Center to Reduce Cancer Health Disparities. "People are dying who should not die, based on what we already know. Delivering what we already know to all American people is the issue," Freeman said.
Pap tests are credited with slashing cervical cancer deaths by 75% in recent decades. This simple $50 test can detect precancerous cells in time to prevent cervical cancer from forming--or, if it's already present, in time to cure this usually slow-growing malignancy. But most invasive cervical cancer is found in women who haven't had a Pap test in five years, if ever.
Poverty is one culprit. Also, women with no regular doctor slip through the cracks. Older women are less likely to get a Pap test, as are recent immigrants, perhaps because of language or cultural issues.
"Cervical cancer shouldn't be a cause of death anymore; in fact, it shouldn't be a problem anymore," said Stephen J. McPhee of the University of California, San Francisco. "Yet here we are in 2005 dealing with a problem that should have been fixed 25 years ago. It's a bad reflection on the U.S. health-delivery system."
With funding from the Centers for Disease Control and Prevention, McPhee started a program in Santa Clara County, Calif., to fight cervical cancer among Vietnamese immigrants, who have the nation's highest incidence of the disease--a rate five times higher than that of white women. Poverty aside, McPhee found that women who saw Vietnamese physicians were half as likely to have ever had a Pap test. Perhaps it's modesty with the usually male doctors, he speculates. But when surveyed, most of those doctors didn't know their patients were at such high risk.
Called Suc Khoe La Vang--"health is gold"--the program advertised Pap tests in Vietnamese, gave Vietnamese doctors classes on cervical cancer, and brought to the county a CDC program that provides free Pap tests for the poor. And it trained volunteer "lay health workers" to educate their friends and neighbors about Pap tests. Overall, the program increased Pap testing significantly, McPhee will report at an American Public Health Association meeting in November. Those lay health workers were particularly influential: Among women who'd never had a Pap test, 46% got one thanks to the volunteers, compared with 27% who only saw ads.
Freeman pioneered another way to use volunteers, as "patient navigators," to help women with an abnormal Pap test result get treated, whether the barrier is money, language, or winding through the complex health care system.
"This is the only person in the health care system whose job it is to watch the entire movement of the patient from funding to resolution," says Freeman, who employs four patient navigators at East Harlem's Ralph Lauren Center for Cancer Care and Prevention.
Among other successes, they get 95% of his center's uninsured patients into a program that will pay for their care.
There is federal money for communities to emulate such programs. A law passed this summer promises $25 million in grants over five years for patient-navigator pilot projects. The CDC's REACH 2010 project is providing another $35 million in grants this year to reduce health disparities in cervical cancer and five other health problems. And in May the government allocated $95 million for 25 community projects aimed at reducing disparities in cervical, breast, and colorectal cancers.
If communities only knew to pay attention to cervical cancer, "this is a really easy one to fix," McPhee says. (AP)
Want more breaking equality news & trending entertainment stories?
Check out our NEW 24/7 streaming service: the Advocate Channel!
Download the Advocate Channel App for your mobile phone and your favorite streaming device!
From our Sponsors
Most Popular
Here Are Our 2024 Election Predictions. Will They Come True?
November 07 2023 1:46 PM
17 Celebs Who Are Out & Proud of Their Trans & Nonbinary Kids
November 30 2023 10:41 AM
Here Are the 15 Most LGBTQ-Friendly Cities in the U.S.
November 01 2023 5:09 PM
Which State Is the Queerest? These Are the States With the Most LGBTQ+ People
December 11 2023 10:00 AM
These 27 Senate Hearing Room Gay Sex Jokes Are Truly Exquisite
December 17 2023 3:33 PM
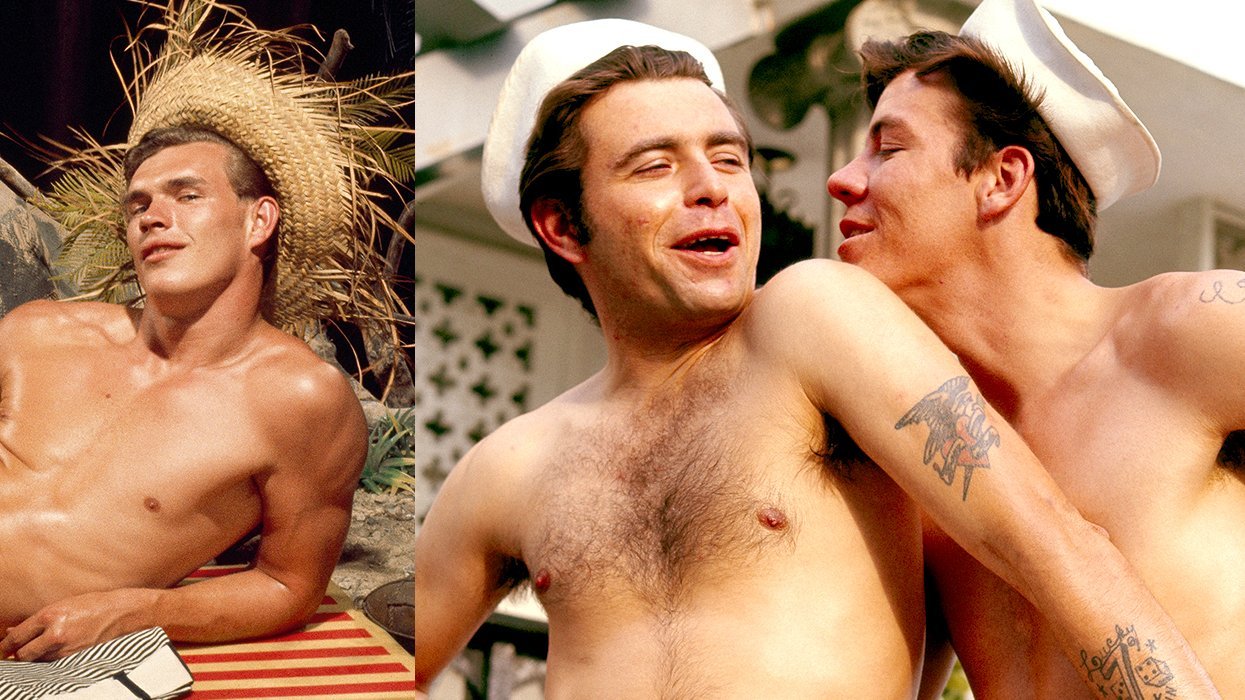
10 Cheeky and Homoerotic Photos From Bob Mizer's Nude Films
November 18 2023 10:05 PM
42 Flaming Hot Photos From 2024's Australian Firefighters Calendar
November 10 2023 6:08 PM
These Are the 5 States With the Smallest Percentage of LGBTQ+ People
December 13 2023 9:15 AM
Here are the 15 gayest travel destinations in the world: report
March 26 2024 9:23 AM
Watch Now: Advocate Channel
Trending Stories & News
For more news and videos on advocatechannel.com, click here.
Trending Stories & News
For more news and videos on advocatechannel.com, click here.
Latest Stories
Supreme Court lets Idaho enforce law criminalizing gender-affirming care for minors
April 15 2024 8:47 PM
Plus
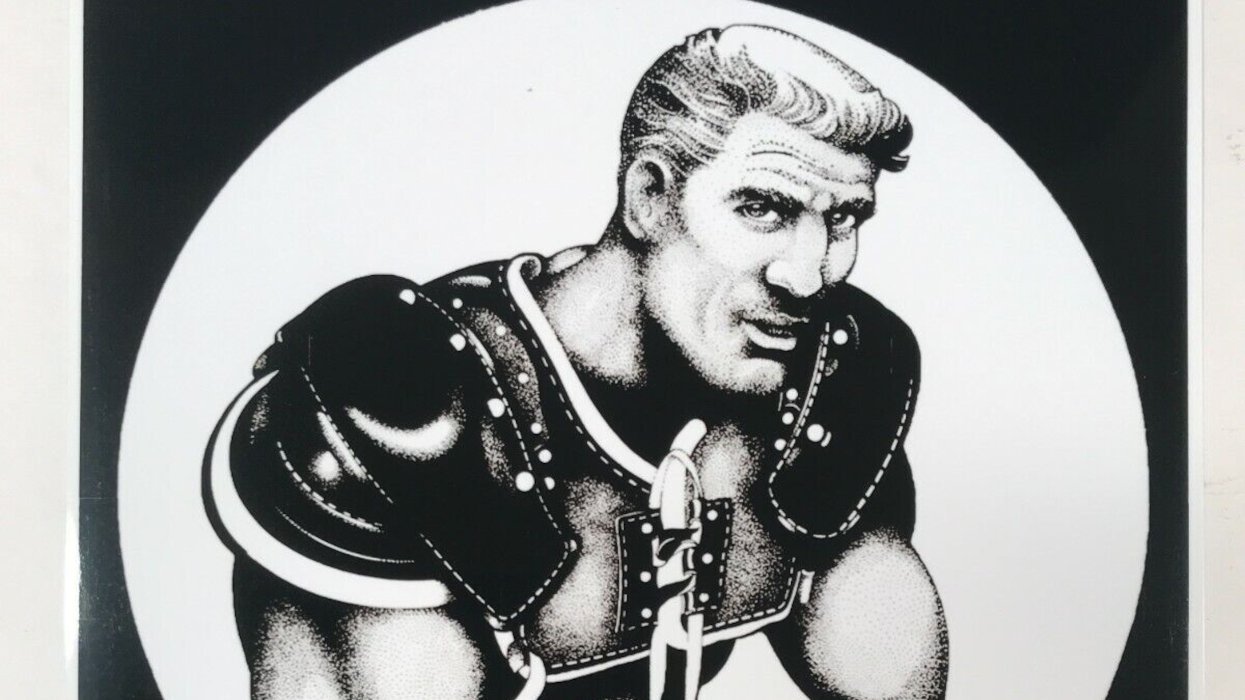
Yahoo FeedGay fetish artist Rex has died — see some of his sexy work
April 15 2024 8:13 PM
Brittney Griner and her wife, Cherelle, are expecting! Here's when baby Griner is arriving
April 15 2024 12:52 PM
Tennessee Senate passes bill making 'recruiting' for trans youth care a felony
April 14 2024 11:17 AM
Trending stories
Most Recent
Recommended Stories for You