CONTACTStaffCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2024 Pride Publishing Inc.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Private Policy and Terms of Use.
Newer mammograms that allow doctors to use digital imaging to help spot cancer are better than standard X-rays for young women and those with dense breasts but not for most postmenopausal women, a landmark study concludes.
Doctors say women who aren't in one of the groups that benefited can skip the extra cost of the newer digital tests and have a standard mammogram. However, they expect digital tests to become more common because of their many advantages, including that they can be stored on a computer and sent electronically whenever a woman moves or a new doctor needs to see them.
"Everything is going filmless. If there's no disadvantage to digital mammography, I would presume over time it will replace film screening," said Kathy Brandt, chief of breast imaging at the Mayo Clinic in Rochester, Minn., who had no role in the study.
The study, funded by the National Cancer Institute, involved 42,760 women in the United States and Canada and was done by the American College of Radiology Imaging Network. Results were to be reported Friday at a medical meeting. They also were released online by the New England Journal of Medicine and will appear in its October 27 edition.
Mammograms cut the risk of breast cancer deaths by up to 35% among women 50 and older but only by 15% to 20% among younger women, who tend to have dense breasts that standard film X-rays have trouble penetrating.
Digital mammograms produce images on a computer screen, where they can be enhanced or magnified to reveal lurking signs of cancer. Doctors have hoped that this would improve mammography's usefulness for younger women.
The study aimed to learn whether they are more accurate; that is, whether they correctly detected cancer and didn't give too many "false alarms."
Each participant received both types of mammograms. Results were reviewed independently by two radiologists, and biopsies settled whether suspicious findings were cancer. Follow-up exams were done a year later to see how many cancers had been missed the first time around. A total of 335 breast cancers were found; both types of mammograms missed about 30% of them. Digital mammograms proved 15% more accurate than standard film X-rays among women under 50, in whom breast cancer is relatively uncommon. Among women with dense breasts and those not yet in menopause, digital mammograms were 11% and 15% better, respectively.
For all other women, "film is just as good," said Etta Pisano, a radiologist at the University of North Carolina at Chapel Hill who led the study. She said the results should help prioritize who gets the more expensive tests: "We don't have enough digital mammography for everyone to get it, and some women won't benefit from it anyway."
The first digital machines came on the U.S. market in 2001, but they account for only 8% of mammography equipment today, largely because of cost. Medicare pays an average of $85.65 for a standard film mammogram and $135.29 for a digital one.
Robert Smith, director of screening at the American Cancer Society, said no woman should delay getting a mammogram if a digital one is not available. The society recommends that annual mammograms start at age 40; the federal government advises them every one to two years for women in their 40s and then annually starting at age 50.
As for the study results, "we'd always like a newer technology to do better in every way," but improving mammograms for certain groups of women is still a gain, he said.
In the study, about two thirds of women either had dense breasts, were under 50, or had not reached menopause. That led Daniel Sullivan, who heads cancer imaging at the National Cancer Institute, to conclude, "It may not be completely representative of the general population" because most mammograms are done on women over 50 who have fatty breasts.
The study was the largest ever done to compare mammography techniques. Earlier studies have found digital mammograms to be comparable in accuracy to film for women in general. (AP)
Want more breaking equality news & trending entertainment stories?
Check out our NEW 24/7 streaming service: the Advocate Channel!
Download the Advocate Channel App for your mobile phone and your favorite streaming device!
From our Sponsors
Most Popular
Here Are Our 2024 Election Predictions. Will They Come True?
November 07 2023 1:46 PM
Meet all 37 of the queer women in this season's WNBA
April 17 2024 11:24 AM
17 Celebs Who Are Out & Proud of Their Trans & Nonbinary Kids
November 30 2023 10:41 AM
Here Are the 15 Most LGBTQ-Friendly Cities in the U.S.
November 01 2023 5:09 PM
Which State Is the Queerest? These Are the States With the Most LGBTQ+ People
December 11 2023 10:00 AM
These 27 Senate Hearing Room Gay Sex Jokes Are Truly Exquisite
December 17 2023 3:33 PM
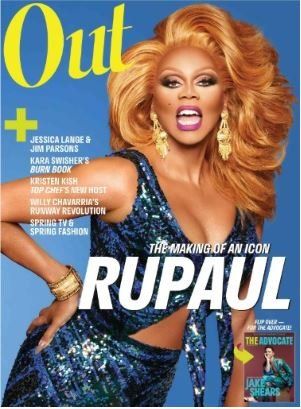
10 Cheeky and Homoerotic Photos From Bob Mizer's Nude Films
November 18 2023 10:05 PM
42 Flaming Hot Photos From 2024's Australian Firefighters Calendar
November 10 2023 6:08 PM
These Are the 5 States With the Smallest Percentage of LGBTQ+ People
December 13 2023 9:15 AM
Here are the 15 gayest travel destinations in the world: report
March 26 2024 9:23 AM
Watch Now: Advocate Channel
Trending Stories & News
For more news and videos on advocatechannel.com, click here.
Trending Stories & News
For more news and videos on advocatechannel.com, click here.
Latest Stories

Pride
Yahoo FeedIndulge in luxury and sensuality with The Pride Store’s Taurus gift guide
April 22 2024 11:46 AM
The gay man leading the Earth Day Initiative offers hope for the future
April 22 2024 9:00 AM
Pattie Gonia takes drag and fierceness to Capitol Hill to voice environmental concerns
April 22 2024 8:23 AM
Jodie Foster leaves her mark in cement at L.A.'s Chinese Theatre
April 22 2024 7:55 AM
Climate change has a bigger impact on LGBTQ+ couples than straight couples. Here's how
April 22 2024 7:42 AM
Iraq postpones vote on bill punishing gay sex with death
April 20 2024 1:31 PM
Russian poetry contest bans entries from transgender poets
April 20 2024 1:25 PM
Here's who won 'RuPaul's Drag Race' season 16
April 20 2024 1:01 PM
The Tip Off: A beginners guide to the WNBA
April 20 2024 11:06 AM
John Fetterman challenges Pa. school board’s cancellation of talk by gay actor
April 19 2024 2:39 PM
New study finds inadequate response to mpox outbreak
April 19 2024 2:06 PM
Fighting back against MAGA’s attacks on equality
April 19 2024 1:00 PM
Just one Christian Nationalist group is behind Idaho's bans on trans care and abortion
April 19 2024 11:57 AM
Trending stories
Most Recent
Recommended Stories for You