CONTACTStaffCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2024 Pride Publishing Inc.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Private Policy and Terms of Use.
The first major study of an experimental vaccine to prevent cervical cancer found it was 100% effective, in the short term, at blocking the disease and lesions likely to turn cancerous, drugmaker Merck said Thursday.
Gardasil, a genetically engineered vaccine, blocks infection by two of the 100-plus types of human papillomavirus, HPV 16 and 18. The two sexually transmitted viruses together cause about 70% of cervical cancers. Other types of HPV also can cause cervical cancer and painful genital or anal warts. About 20 million Americans have some form of HPV.
The final-stage study of Gardasil included 10,559 sexually active women ages 16 to 26 in the United States and 12 other countries who were not infected with HPV 16 or 18. Half got three vaccine doses over six months; half got dummy shots. Among those still virus-free after the six months, none who received the vaccine developed cervical cancer or precancerous lesions over an average two years of follow-up, compared with 21 who got dummy shots.
"To have 100% efficacy is something that you have very rarely," said Eliav Barr, Merck's head of clinical development for Gardasil. "We're breaking out the champagne."
The study, which was funded by Merck, was to be presented Friday at a meeting of the Infectious Diseases Society of America.
A second analysis, including hundreds more women participating in the ongoing study, showed that after just one dose the vaccine was 97% effective. That analysis found only one of the 5,736 women who got the vaccine developed cervical cancer or precancerous lesions, compared with 36 among the 5,766 who got dummy shots. Barr said the 97% rate was more "real world," given that patients sometimes miss or delay follow-up shots or tests.
"I see this as a phenomenal breakthrough," said Gloria Bachmann, director of the Women's Health Institute at Robert Wood Johnson Medical School in New Brunswick, N.J. Bachmann said diagnosis of infection leaves women anxious over the heightened risk of cervical cancer and raises questions among couples about infidelity and prior sexual activity.
"You have to get students [vaccinated] in grammar school, middle school, high school before they become sexually active," she said.
Cervical cancer is the second most common cancer in women and their number 2 cause of cancer deaths, resulting in about 3,000 deaths in the United States and nearly 300,000 around the world each year. At least half of sexually active men and women become infected with HPV at some point.
The immune system clears most such infections in a year or two, but several types of HPV can persist, cause cervical cancer, or trigger other cancers in the genital area. There is no cure for HPV, but the cancers can be treated, and an improved Pap test is catching more cervical cancer before it has spread.
Whitehouse Station, N.J.-based Merck is seeking to beat rival drugmaker GlaxoSmithKline to market with the first cervical cancer vaccine. GlaxoSmithKline did not return a call seeking comment but has published research showing its vaccine against HPV 16 and 18 prevents persistent HPV infection. The Merck vaccine also reduces infection with HPV 6 and 11, which cause 90% of genital warts cases.
Merck plans by year's end to seek Food and Drug Administration approval to sell its vaccine for use by girls and young women. "If all goes well, sometime in 2006 it should be on the market," Barr said.
Merck is continuing research on Gardasil and will soon report on four years of follow-up on women in the current study. The company also will explore whether the vaccine's effectiveness wanes over time. Barr noted that some women in the study developed dangerous precancerous lesions caused by HPV types other than 16 and 18. (AP)
Want more breaking equality news & trending entertainment stories?
Check out our NEW 24/7 streaming service: the Advocate Channel!
Download the Advocate Channel App for your mobile phone and your favorite streaming device!
From our Sponsors
Most Popular
Here Are Our 2024 Election Predictions. Will They Come True?
November 07 2023 1:46 PM
Meet all 37 of the queer women in this season's WNBA
April 17 2024 11:24 AM
17 Celebs Who Are Out & Proud of Their Trans & Nonbinary Kids
November 30 2023 10:41 AM
Here Are the 15 Most LGBTQ-Friendly Cities in the U.S.
November 01 2023 5:09 PM
Which State Is the Queerest? These Are the States With the Most LGBTQ+ People
December 11 2023 10:00 AM
These 27 Senate Hearing Room Gay Sex Jokes Are Truly Exquisite
December 17 2023 3:33 PM
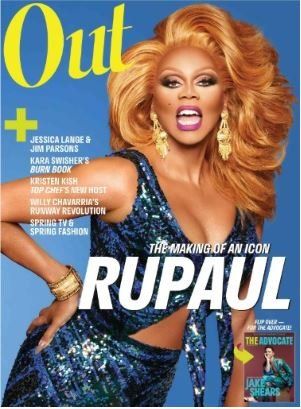
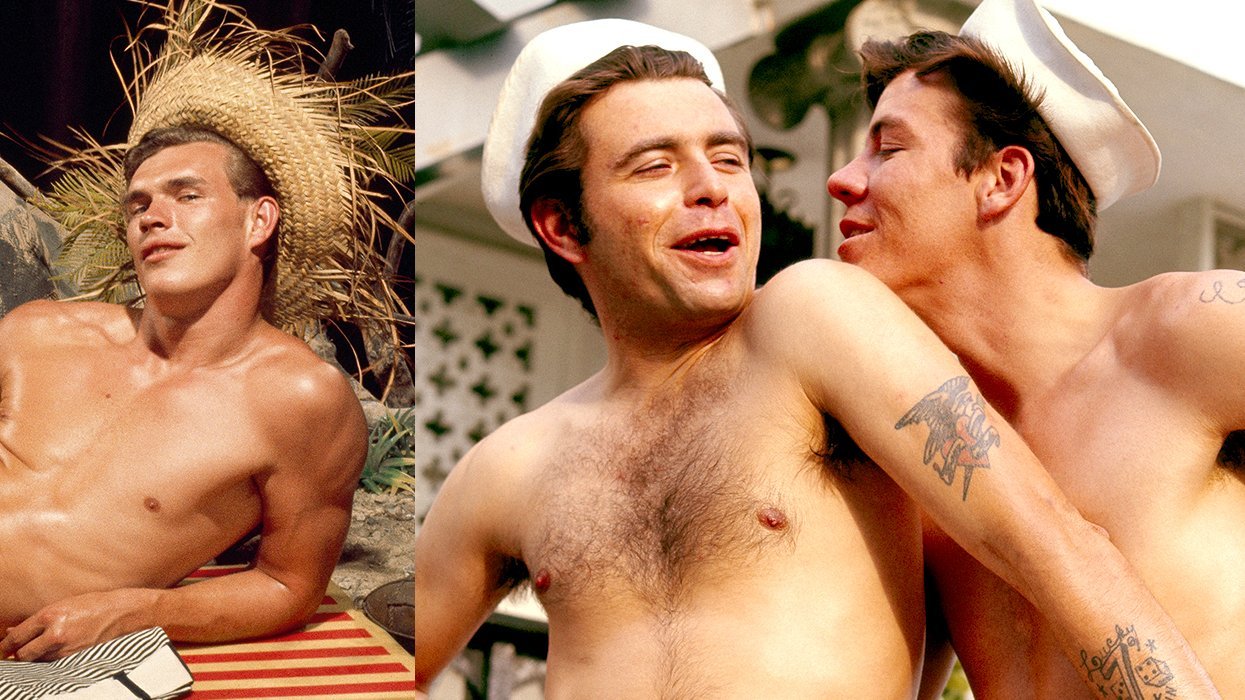
10 Cheeky and Homoerotic Photos From Bob Mizer's Nude Films
November 18 2023 10:05 PM
42 Flaming Hot Photos From 2024's Australian Firefighters Calendar
November 10 2023 6:08 PM
These Are the 5 States With the Smallest Percentage of LGBTQ+ People
December 13 2023 9:15 AM
Here are the 15 gayest travel destinations in the world: report
March 26 2024 9:23 AM
Watch Now: Advocate Channel
Trending Stories & News
For more news and videos on advocatechannel.com, click here.
Trending Stories & News
For more news and videos on advocatechannel.com, click here.
Latest Stories
Trans man Tee Arnold shot to death in Florida
April 17 2024 4:41 PM
Can scientific research on the causes of homosexuality be used against LGBTQ+ people?
April 17 2024 4:02 PM
George Takei releases kids' book about his childhood in internment camp
April 17 2024 3:18 PM

PLUS
ExclusivesTodrick Hall on surviving the rumors and remembering where he came from
April 17 2024 2:33 PM

Pride
Yahoo FeedHow The Pride Store celebrates National Tea Day: A tale of two brews
April 17 2024 2:14 PM
'Parents' Rights' movements forget families have the right to read LGBTQ+ books
April 17 2024 10:15 AM
This gay man had to flee Ghana after a violent attack. He’s finally been granted asylum
April 17 2024 9:17 AM
Trending stories
Most Recent
Recommended Stories for You