CONTACTStaffCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2024 Pride Publishing Inc.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Private Policy and Terms of Use.
It's an Achilles' heel of HIV therapy: The AIDS virus can sneak into the brain to cause dementia, despite today's best medicines.
Now scientists are beginning to test drugs that may protect against the memory loss and other symptoms of so-called neuroAIDS, which afflicts at least one in five people with HIV and is becoming more common as patients live longer.
With nearly 1 million Americans, and nearly 40 million people worldwide, living with HIV, that's a large and under-recognized toll.
"That means HIV is the commonest cause of cognitive dysfunction in young people worldwide," says Justin McArthur, vice chairman of neurology at Baltimore's Johns Hopkins University, who treats neuroAIDS. "There's no question it's a major public-health issue."
While today's most powerful anti-HIV drugs do help by suppressing levels of the virus in blood--so that there's less to continually bathe the brain--they can't cure neuroAIDS. Why? HIV seeps into the brain very soon after someone is infected, and few anti-HIV drugs can penetrate the brain to chase it down.
"Despite the best efforts of (anti-HIV) therapy, brain is failing," says Harris Gelbard, a neurologist at the University of Rochester Medical Center. He is part of a major new effort funded by the National Institutes of Health to find the first brain-protecting treatments.
What's now called neuroAIDS is much different from the AIDS dementia of the epidemic's early years, when patients often had horrific brain symptoms similar to end-stage Alzheimer's, unable to move or talk. They'd die within six months.
Today, anti-HIV medication has resulted in a more subtle dementia that strikes four years or more before death: At first patients forget phone numbers and their movements slow. They become less able to juggle multiple tasks.
Some worsen until they can't hold a job or perform other activities, but not everyone worsens--and doctors can't predict who will. In a vicious cycle, the memory loss makes many forget their anti-HIV pills, so the virus rebounds.
Gelbard estimates that neuroAIDS reduces patients' mental function by 25%.
If HIV patients live long enough, many specialists worry, nearly all of them may suffer at least some brain symptoms.
"They're living longer with HIV in the brain," explains Kathy Kopnisky of the NIH's National Institute of Mental Health, which is spending about $60 million investigating neuroAIDS. "And they're aging, so they're going through the normal brain aging-related processes" that can make people vulnerable to Alzheimer's and other brain diseases.
Biologically, this is a different type of dementia from any caused by Alzheimer's or Parkinson's, and drugs for those brain-degenerating diseases so far are proving disappointing against neuroAIDS.
So the government-funded attack has two fronts:
- First, to figure out which of the powerful anti-HIV cocktails are the best bet for HIV patients with memory problems.
A few of today's HIV-suppressing drugs, such as nevirapine, abacavir, AZT, and indinavir, can penetrate the blood-brain barrier, says Ron Ellis, MD, of the University of California, San Diego.
But no one knows if using those drugs instead of others will slow the brain damage once neuroAIDS symptoms begin. Early next year Ellis will begin a study of 120 such patients--at UCSD, Johns Hopkins, and Washington University in St. Louis--to try to tell, by randomly assigning them to either a brain-penetrating cocktail or different drugs.
- Second, to find drugs that protect nerve cells from the inflammation-triggered toxic chain reaction that seems to be how HIV wreaks its damage.
Topping the candidates are the epilepsy drug valproic acid and lithium, a drug long used in manic depression. Both inhibit an enzyme, called GSK-3b. The body normally makes the enzyme, but too much is poisonous. In the brain, HIV knocks that careful balancing act out of whack, leading to death of connections key to memory and other neuronal functions.
In a recent pilot study, Gelbard found tantalizing signs that valproic acid might increase brain connections in a few neuroAIDS patients, and improve their symptoms. He's about to begin a second-stage study to try to tell if the effect is real; a similar pilot trial with lithium is under way.
Seeking a one-two punch, Gelbard also hopes to soon begin a human study of an experimental drug that targets a second inflammatory protein HIV uses to trigger brain cells to kill themselves. (Lauran Neergaard, AP)
Want more breaking equality news & trending entertainment stories?
Check out our NEW 24/7 streaming service: the Advocate Channel!
Download the Advocate Channel App for your mobile phone and your favorite streaming device!
From our Sponsors
Most Popular
Here Are Our 2024 Election Predictions. Will They Come True?
November 07 2023 1:46 PM
Meet all 37 of the queer women in this season's WNBA
April 17 2024 11:24 AM
17 Celebs Who Are Out & Proud of Their Trans & Nonbinary Kids
November 30 2023 10:41 AM
Here Are the 15 Most LGBTQ-Friendly Cities in the U.S.
November 01 2023 5:09 PM
Which State Is the Queerest? These Are the States With the Most LGBTQ+ People
December 11 2023 10:00 AM
These 27 Senate Hearing Room Gay Sex Jokes Are Truly Exquisite
December 17 2023 3:33 PM
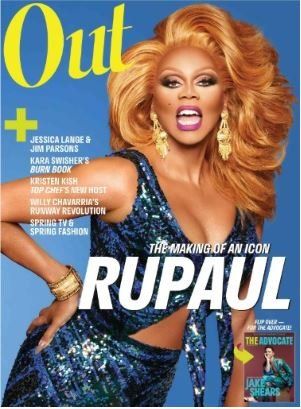
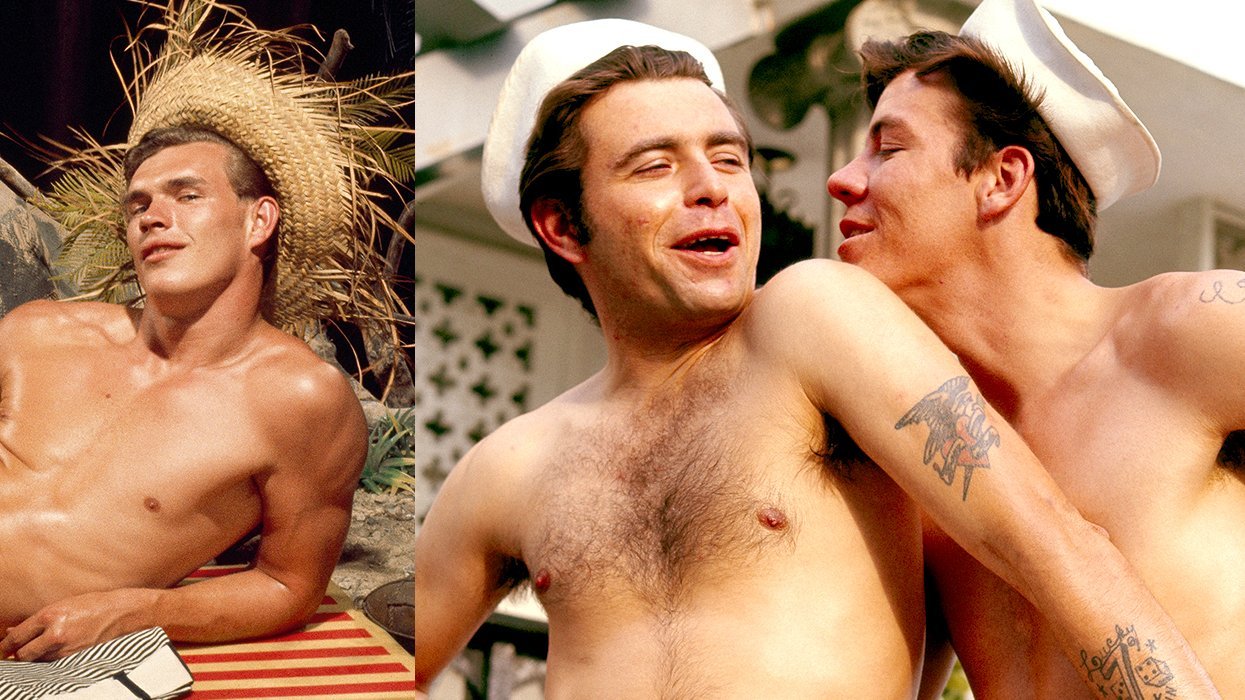
10 Cheeky and Homoerotic Photos From Bob Mizer's Nude Films
November 18 2023 10:05 PM
42 Flaming Hot Photos From 2024's Australian Firefighters Calendar
November 10 2023 6:08 PM
These Are the 5 States With the Smallest Percentage of LGBTQ+ People
December 13 2023 9:15 AM
Here are the 15 gayest travel destinations in the world: report
March 26 2024 9:23 AM
Watch Now: Advocate Channel
Trending Stories & News
For more news and videos on advocatechannel.com, click here.
Trending Stories & News
For more news and videos on advocatechannel.com, click here.
Latest Stories
Black trans woman África Parrilla García shot to death in Puerto Rico
April 18 2024 4:55 PM
Marjorie Taylor Greene has sunk so low even Fox News can't stand her anymore
April 18 2024 4:04 PM
Single lesbians are avoided by straight women, but not straight men. Here's why.
April 18 2024 3:18 PM
The LGBTQ+ movie fan's guide to the 2024 TCM Classic Film Festival
April 18 2024 2:44 PM
The federal government failed on mpox. Ritchie Torres's new bill addresses that (exclusive)
April 18 2024 1:21 PM
True
In the face of tweets and turmoil, why I left the South as a medical student
April 18 2024 7:30 AM
Trans man Tee Arnold shot to death in Florida
April 17 2024 4:41 PM
Can scientific research on the causes of homosexuality be used against LGBTQ+ people?
April 17 2024 4:02 PM
Trending stories
Most Recent
Recommended Stories for You