Drug-resistant
staph infections that have made headlines in recent weeks
come from what the nation's top doctor calls ''the cockroach
of bacteria'' -- a bad germ that can lurk in lots of
places but not one that should trigger panic.
''This isn't
something just floating around in the air,'' Dr. Julie
Gerberding, head of the Centers for Disease Control and
Prevention, told members of Congress on Wednesday.
It takes close
contact -- things like sharing towels and razors, or
rolling on the wrestling mat or football field with open
scrapes, or not bandaging cuts -- to become infected
with the staph germ called MRSA outside of a hospital,
she said. But MRSA is preventable largely by
common-sense hygiene, Gerberding stressed.
''Soap and water
is the cheapest intervention we have, and it's one of
the most effective,'' she told a hearing of the House
Committee on Oversight and Government Reform.
At issue is
methicillin-resistant Staphylococcus aureus, a
form of the incredibly common staph family of germs. About
one in every three people carries staph aureus in their
noses. In about 1 million people, the type they carry
is MRSA.
''I like to think
of it as the cockroach of bacteria,'' Gerberding said,
pointing out MRSA's ability to live on various surfaces and
spread by catching a ride on an unwashed hand.
Over time, germs
evolve to withstand treatment. Most staph is no longer
treatable by the granddaddy of antibiotics, penicillin. By
the 1960s, staph also began developing resistance to a
second antibiotic, methicillin.
So MRSA is not a
new problem. What is new is public anxiety about it.
MRSA mostly
causes skin infections such as boils and abscesses. But it
can sometimes spread to cause life-threatening blood
infections. Last month the CDC reported the first
national estimate of serious MRSA infections -- 94,000
a year. It's not clear how many people die, but one
estimate put the MRSA death toll at more than 18,000,
slightly higher than U.S. deaths from AIDS.
There are two
distinct strains of MRSA, a type spread in hospitals and
other health facilities and a genetically different type
spread in communities. The vast majority of victims
are hospital patients; only 14% of serious MRSA
infections are the kind spread in the community.
But the CDC's
report coincided with the death of a 17-year-old Virginia
high school student, prompting a spate of reports of MRSA
infections in schools. That prompted lawmakers to
pepper Gerberding with questions Wednesday:
-Should schools
close for cleaning if a student gets MRSA? That's not
medically necessary, Gerberding said. Bleach and a list of
other germicides can be used in routine cleaning of
areas and equipment where bacteria cluster.
''There's no need
to go in and disinfect a whole school because that
isn't how this organism is transmitted,'' she said.
-How worried
should parents be? Some 200 children a year will get serious
MRSA, and the vast majority will be treated successfully,
Gerberding said. Community-spread MRSA is still easily
treated by many other routine antibiotics. So wash and
bandage cuts and seek prompt medical care if they show
signs of infection.
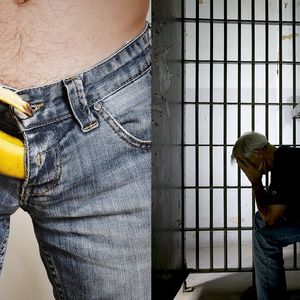
Most outbreaks of
community-spread MRSA occur not in schools but in
prisons, where inmates share toiletries and lack or don't
use soap.
-Should every
patient entering a hospital be tested for MRSA, and
isolated if they harbor it? Some hospitals have begun that,
but current guidelines call for that step only if
hospitals fail to reduce MRSA infections by less
drastic means, Gerberding said.
Her concern:
''Patients in isolation get less care.'' Doctors and nurses
check on them less. They get more bed sores, opening the
body to other life-threatening germs.
There is a
biological conundrum: Hospital-based MRSA is more common and
vulnerable to fewer antibiotics than the strain spread in
communities, and already-ill patients are more likely
to die from it. Yet the community strain of MRSA may
be somewhat stronger, possibly explaining why
otherwise healthy people sometimes succumb.
It's a strain
called USA300, and if it penetrates the skin, it can cause
key immune cells -- white blood cells -- to explode, setting
off a chain reaction of inflammation, Gerberding
explained. This strain, unlike most hospital MRSA,
also produces a toxin known as PVL, and scientists are
furiously investigating its role.
New antibiotics
are important but won't solve MRSA or the myriad other
drug-resistant bacteria, she said.
Germs ''will
always be one step ahead of our drugstores,'' Gerberding
said. ''We have to get back to the basics'' -- wash your
hands and cover your cuts. (AP)