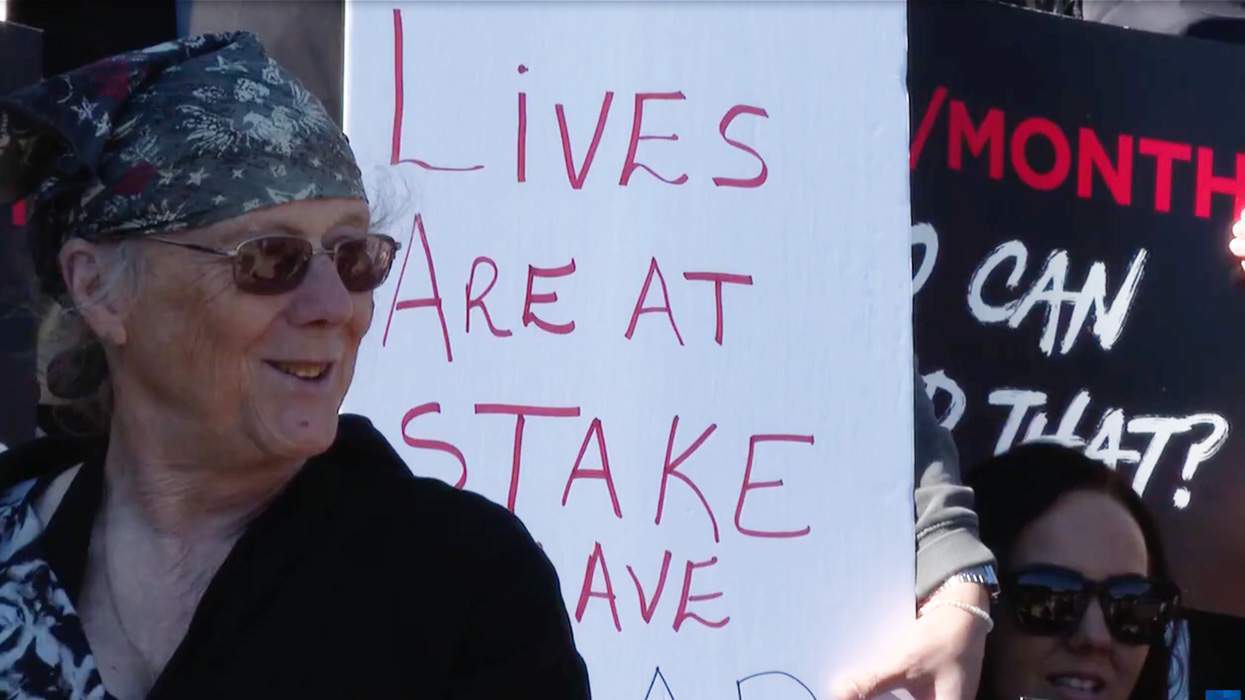
As understanding about the lives and experiences of transgender people grows in our society, access to comprehensive, gender-affirmative health care is also increasing. For example, in the U.S., the Affordable Care Act bans discrimination in health care coverage based on gender identity and expression. Last June the federal government did away with Medicare's 33-year-old blanket exclusion of coverage for gender reassignment surgery. That same month my home state of Massachusetts followed in the footsteps of five other states and the District of Columbia in requiring public and private health insurers to cover transgender-related health care services, including cross-sex hormone therapy and surgery.
That's the good news.
The bad news is that just because more transgender people now have health care coverage and access to care, doesn't mean they are actually getting the preventive health services they need. Our research at the Fenway Institute at Fenway Health suggests that more than one in three trans men who are patients are not up to date on cervical cancer screening and many are not getting routine screening for sexually transmitted infections.
This is not surprising. We know that it is difficult for FTM patients to find health care providers who are knowledgeable about health issues specific to transgender people, and can talk about sexual health in sensitive and gender-affirming ways. Transphobia is also a significant factor in health care lapses, especially where sexual health is concerned. We have made inroads on ensuring access to care since Robert Eads succumbed to ovarian cancer in 1999 after dozens of doctors refused him treatment because he was transgender, as chronicled in the documentary film Southern Comfort. But too many transgender men are still turned away or receive substandard care simply because of their gender identity and expression.
The groundbreaking National Transgender Discrimination Survey found that a little less than one-third (28 percent) of survey respondents had delayed seeking care for fear of experiencing discrimination. In a secondary analysis of data from that survey that included more than 2,500 transgender men in the U.S., I found that more than one-third (39 percent) of transgender men reported postponing or avoiding preventive health care because they feared discrimination. Meanwhile, more than one in 10 transgender men (14 percent) reported being denied services or refused care because of their transgender status. (This analysis will be presented at the American Public Health Association Annual Meeting and Expo later this month.)
The Fenway Institute, in collaboration with the World Professional Association for Transgender Health and the Center of Excellence for Transgender Health at the University of California, San Francisco, is preparing to launch a two-year research project aimed at finding new strategies of care that could potentially lead to alternative cervical cancer screening strategies and less invasive STI detection practices for FTMs.
With a grant from the independent nonprofit Patient-Centered Outcomes Research Institute we will be studying the sexual health of transgender men for the first time ever. Working with this community's members, providers, and key stakeholders, we will investigate the prevalence of sexually transmitted infections among trans men and focus on innovations in preventive sexual health screening in those patients who are sexually-active.
The project is designed to fill key gaps in clinical knowledge about sexual health in trans men by comparing the effectiveness of alternative strategies for sexual health prevention, screening, and diagnosis. This will include evaluating the acceptability and effectiveness of having patients perform self-swab testing for human papillomavirus, or HPV, the primary cause of cervical cancer, and a health concern about which no clinical data in these patient populations currently exists. We're excited to test an HPV screening method that empowers patients to take control of their sexual health.
This PCORI grant is a major and unprecedented investment in the health and well-being of transgender men. It recognizes important and difficult dimensions of their lives and seeks workable solutions.
If we are able to find strategies that will increase preventive sexual health screenings in transgender men, the possibility exists that these strategies can also be employed with other population groups experiencing low rates of preventive screening. Meanwhile, the simple act of investment in this research represents a major step forward in transgender health and toward achieving greater health equity for transgender men.
SARI REISNER is a research scientist at the Fenway Institute and a postdoctoral research fellow in the Department at Epidemiology at Harvard School of Public Health.











Charlie Kirk DID say stoning gay people was the 'perfect law' — and these other heinous quotes
These are some of his worst comments about LGBTQ+ people made by Charlie Kirk.