
CONTACTAbout UsCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2025 Equal Entertainment LLC.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Privacy Policy and Terms of Use.
We need your help
Your support makes The Advocate's original LGBTQ+ reporting possible. Become a member today to help us continue this work.
Your support makes The Advocate's original LGBTQ+ reporting possible. Become a member today to help us continue this work.
A new study indicating that antiretroviral medication is effective in preventing HIV may be raising as many questions as it has answered.
Among them: Who will pay for it? Who should take it? And will it lead to less condom use among gay men?
"It's an incredible biologic success with incredible behavior challenges," Mitchell Warren, executive director of the AIDS Vaccine Advocacy Coalition, said of the study, published Tuesday in The New England Journal of Medicine.
Funded by the National Institutes of Health and the Bill and Melinda Gates Foundation and involving nearly 2,500 gay men -- as well as transgender women who have sex with men -- the three-year study found that those who were given the antiretroviral pill Truvada were 44% less likely to become infected with HIV than those who received a placebo.
When participants took the medication as directed 90% of the time -- verified through blood tests --Truvada was 73% effective in preventing infection. All study subjects received HIV testing and safer-sex counseling every four weeks.
Though "pre-exposure prophylaxis," or PrEP, is not new, the study is the first large-scale look at a prevention method that is expensive and unavailable to many.
White House officials quickly praised the study results as encouraging, though hardly a replacement for established methods of HIV prevention, including proper condom use. In a statement to The Advocate, Jeffrey S. Crowley, director of the White House Office of National AIDS Policy, said that further research on PrEP must include women and other groups.
"ONAP recognizes that one study is not definitive and this single study was focused on one population," Crowley said.
Researchers at the National Institutes of Health, the Centers for Disease Control and Prevention, and the U.S. Agency for International Development "have been active participants in a global effort to examine this issue in different populations and answer other critical questions in order for us to know how to use these findings as part of a comprehensive, evidence-based approach to HIV prevention," Crowley added.
Implementing PrEP as an effective HIV prevention tool presents many challenges. Getting at-risk individuals to take medication consistently is one of them: Truvada can initially cause minor side effects such as nausea, while long-term health complications resulting from the toxicity of antiretroviral drugs remain a concern.
"This data is exciting, but it only begins to tell a story. We don't know how to sustain PrEP as a regimen," AVAC's Warren said. "It's not unlike the situation with condoms. They're effective when people use them correctly and consistently. This pill doesn't change that."
It's also unclear what dosage is most effective -- and practical for general use. "We may find that we don't need daily use," said Cornelius Baker, a senior HIV/AIDS adviser at the AED Center on AIDS and Community Health and a member of the Presidential Advisory Council on HIV/AIDS. "Maybe there are strategies for intermittent use. Even people who were 50% adherent [in the study] were still seeing a benefit. ... We still need to know what the real-world implications are."
Other experts said that PrEP treatment is simply not a viable option for most people in the near term, with funding for HIV/AIDS care and outreach in the U.S. facing continued setbacks.
"It's not available from a very practical perspective," AIDS Project Los Angeles executive director Craig E. Thompson said of PrEP, though he lauded the study and its potential implications for further research and future prevention efforts. "If you're a gay man who's not infected, I don't know where you would go to get these drugs. There's not an agency in the country that subsidizes it. Is insurance going to pay for an HIV-negative person's medication?"
PrEP may be most effectively implemented in communities with higher risk of infection and lower rates of condom use, Thompson said, including sex workers, who are often paid more money for engaging in unprotected sex.
And although the drugs that make up Truvada are less likely than some other meds to cause a drug-resistant strain of HIV to develop, some wonder about the risk that a person who contracts HIV while taking the medication as PrEP can transmit a Truvada-resistant strain to a sexual partner.
"Would I recommend someone [use PrEP]? It's a personal decision," said Robert Gallo, director of the Institute of Human Virology at the University of Maryland School of Medicine. "If you're taking the drug, and you're [healthy] now, you don't know the long-term effects. You don't know if you're going to create a drug-resistant variant."
As far as who might pay for the medication -- insurance companies, drug companies, government agencies -- Baker said it's too early to speculate, though HIV prevention likely remains less costly than treating those already infected with the virus.
From our Sponsors
Most Popular
Bizarre Epstein files reference to Trump, Putin, and oral sex with ‘Bubba’ draws scrutiny in Congress
November 14 2025 4:08 PM
True
Jeffrey Epstein’s brother says the ‘Bubba’ mentioned in Trump oral sex email is not Bill Clinton
November 16 2025 9:15 AM
True
Gay makeup artist Andry Hernández Romero describes horrific sexual & physical abuse at CECOT in El Salvador
July 24 2025 10:11 AM
True
Watch Now: Pride Today
Latest Stories
Democratic officials sue RFK Jr. over attempt to limit gender-affirming care for trans youth
December 24 2025 4:30 PM
Heated Rivalry season 2: Everything we know so far
December 24 2025 3:30 PM
Lillian Bonsignore will be first out gay Fire Department of New York commissioner
December 23 2025 6:21 PM
The HIV response on a cliff-edge: advocacy must drive urgent action to end the epidemic
December 23 2025 2:23 PM
CECOT story pulled by Bari Weiss gets viewed anyway thanks to Canadian streaming service
December 23 2025 2:05 PM
Burkina Faso issues first sentence for 'homosexuality and related practices'
December 23 2025 2:02 PM
Transgender NSA employee files discrimination lawsuit against Trump administration
December 23 2025 12:03 PM
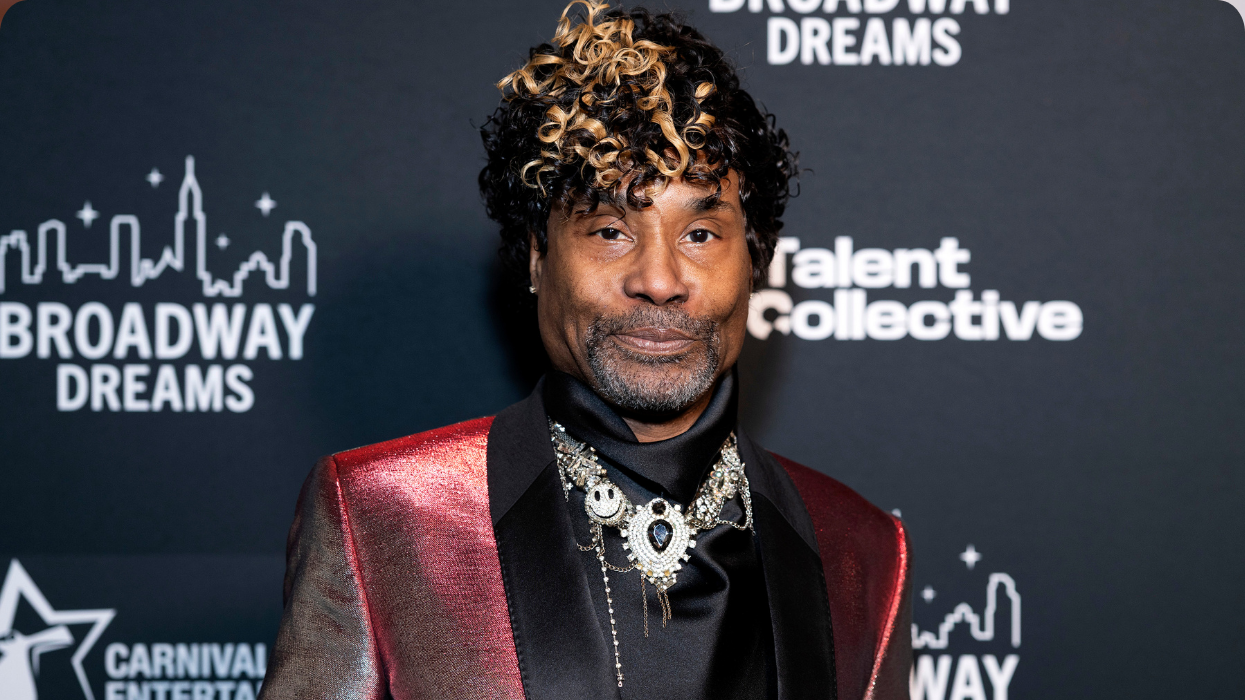
Billy Porter is set to make a 'full recovery' from sepsis
December 23 2025 11:54 AM
Soccer stars Rafaelle Souza and Halie Mace are engaged & the video is so adorable
December 23 2025 10:52 AM
What is 'hopecore' and how can it make life better for LGBTQ+ people?
December 23 2025 10:00 AM
Santa Speedo Run 2025: See 51 naughty pics of the festive fundraiser
December 23 2025 6:00 AM
Instructor who gave U of Oklahoma student a zero on anti-trans paper removed from teaching
December 22 2025 9:36 PM
All about the infamous CECOT prison — on which CBS's Bari Weiss pulled a story
December 22 2025 7:27 PM
Chest binder vendors respond to 'absurd' FDA warning letter: 'Clearly discrimination'
December 22 2025 3:16 PM
Gay NYC Council member Erik Bottcher drops U.S. House bid, will run for state Senate instead
December 22 2025 2:03 PM
Massachusetts removes rule requiring foster parents to support LGBTQ+ youth
December 22 2025 12:55 PM
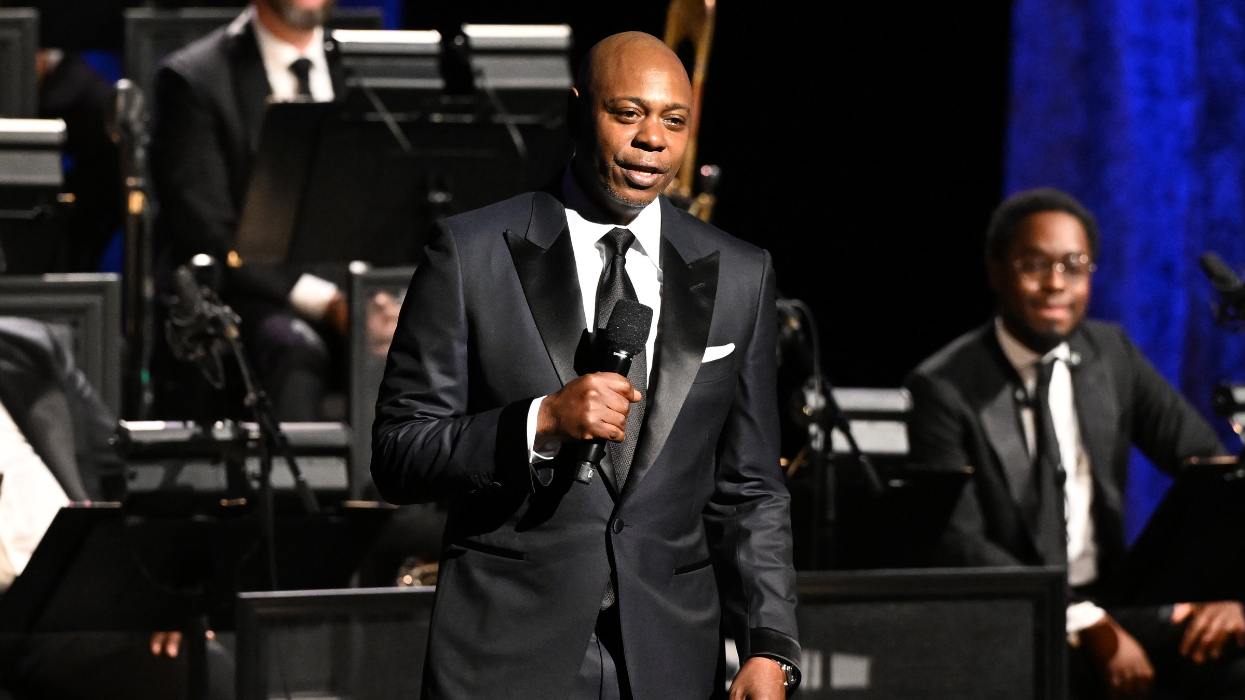
Dave Chappelle defends Saudia Arabia set: Trans jokes 'went over very well'
December 22 2025 12:33 PM
Texas judge who refused to officiate same-sex weddings sues to overturn marriage equality
December 22 2025 11:41 AM
Trending stories
Recommended Stories for You


































































Charlie Kirk DID say stoning gay people was the 'perfect law' — and these other heinous quotes