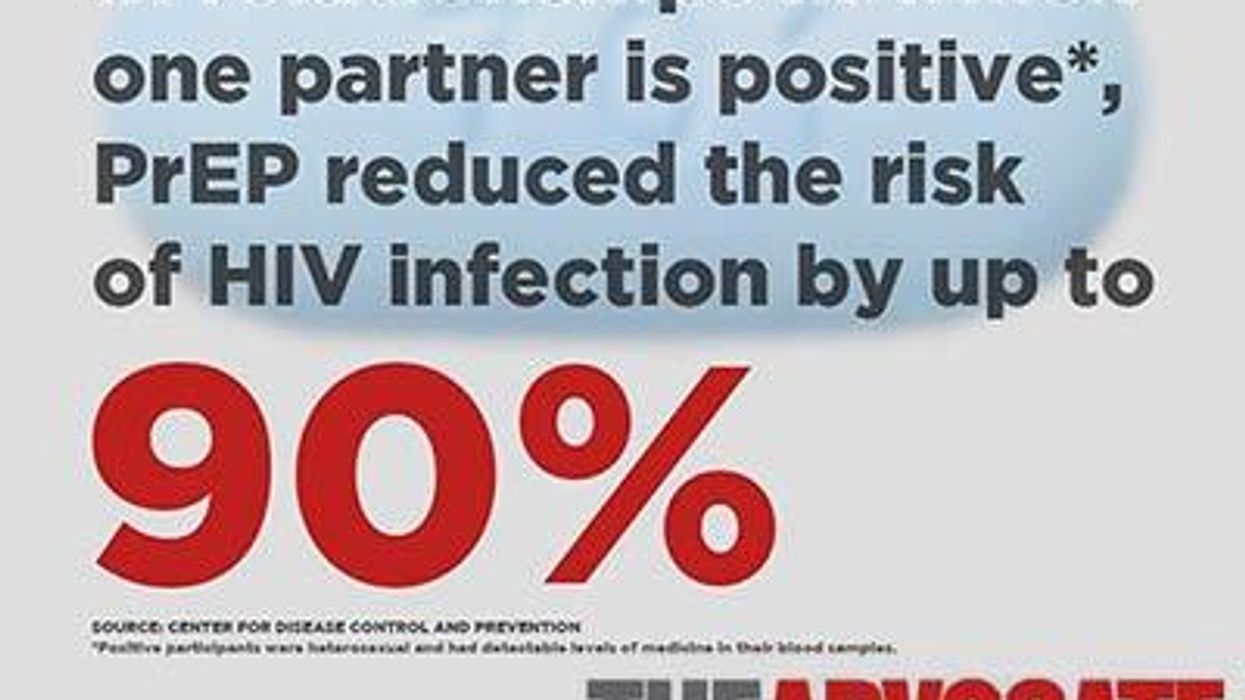
By now you know that studies have shown that the use of Truvada as PrEP to prevent HIV infection is safe and effective. When taken once daily as prescribed by your doctor, PrEP has been shown to be 99 percent effective at preventing HIV infection, regardless of whether a condom is used. With less than optimal use, efficacy drops down to the mid-70s.
Experts throughout the field have stressed that PrEP is an important new weapon in the ongoing battle against HIV and AIDS. You'd think with all the attention focused on this latest development in prevention that PrEP is the tool that will finally bring about an end to new HIV transmissions.
Unfortunately, it's not quite that simple, say several experts in the field.
"No intervention is a stand-alone answer to ending HIV transmission," says Demetre C. Daskalakis, assistant commissioner for the New York City Department of Health and Mental Hygiene's Bureau of HIV/AIDS. "PrEP may protect individuals at risk from infection, but more precisely, it may prevent acute HIV infection, the earliest and most infectious stage of HIV."
In fact, most doctors and activists -- in addition to overarching agencies like the Centers for Disease Control and Prevention and the World Health Organization -- urge that PrEP be used in conjunction with existing strategies (including condom use and regular testing) to minimize the risk of contracting HIV, especially for those who fall into one of several high-risk categories.
Experts say while it may not be the end-all, be-all in the ongoing fight against HIV, PrEP does provide an important new tool in that fight. Among a community that has for nearly 30 years preached the singular gospel of condom use, a change in tune -- or more accurately, a harmony added to that ongoing chorus -- could have a substantial impact.
"PrEP is a prevention game-changer because it allows us to offer more than one item on our HIV prevention menu," explains Daskalakis. "Now we can offer PrEP with the knowledge that it may provide the right type of protection for a person unable or unwilling to adhere to regular condom use."
Diane Havlir, a leading AIDS researcher, PrEP supporter, and professor at the University of California, San Francisco's School of Medicine, agrees with Daskalakis -- then goes a step further to implicate PrEP in a broader paradigm-shift that has expanded the definition of "treatment as prevention" to apply beyond giving medication to HIV-positive people to reach undetectable viral loads so they can no longer transmit the virus, to giving medication to negative people that keeps them from ever aquiring HIV.
"Combination HIV prevention is the game-changer," she says. "PrEP is one component of combination prevention -- we need to facilitate and optimize its use."
New York governor Andrew Cuomo this month announced a plan to do just that. Ambitiously titled the "End of AIDS" Task Force, the initiative seeks to end new HIV infections in New York by 2020.
New York-based Daskalakis confirms that PrEP is a crucial part of the governor's plan to end AIDS, again positioning the strategy as one cog in a machine of treatment and prevention.
"PrEP is part of a combination attack on the HIV epidemic," explains Daskalakis. "By identifying people with HIV and linking them to care, treating those with HIV, and offering PrEP to those at risk, we have a strategy that will drive down new HIV infections below epidemic levels." (For New York, that would mean reducing new infections from 3,000 annually to around 750, on par with that of new tuberculosis cases and below the average number of AIDS-related deaths in the state, according to The New York Times.)
Lauding Cuomo's plan as an effective translation of "cutting-edge science directly into public health implementation," Daskalakis says New York's model is one that should be readily followed by other cities and states.
Bringing the rate of new infections -- which have been skyrocketing among key risk groups like young gay and bisexual men -- "below epidemic levels" could prove to be the critical turning point in ultimately closing this chapter in history where HIV and AIDS represent an unmanageable virus that can only be contained, not conquered.
When asked if she believes it's possible to forsee a future generation that is free of HIV, Havlir stresses that it's not a matter of whether such a future is possible, but rather how quickly we can arrive at such a reality.
"We have evidence-based interventions that can dramatically reduce the number of new HIV infections, and suffering and death from this disease," she explains. "The pace that we reach an HIV-free generation will be defined by our actions now -- how we ensure that infected persons receive optimal therapy and how persons at risk remain free from HIV."
Havlir is not only one of the nation's leading HIV researchers, with clinical experience dating back to the earliest days of the epidemic, she is also the founder of San Francisco's "Getting to Zero" consortium, which aims to connect providers, researchers, and at-risk individuals to prevent and treat all HIV in San Francisco. The combination of improved testing methods leading to early (and improved) treatment for those who are HIV-positive, combined with PrEP to reduce the number of new infections -- not to mention the increasing potential of an actual cure -- has Havlir optimistic.
"For the first time ever -- we've never really said this before -- we think we can begin to end AIDS," she told The Advocate earlier this year.
While PrEP may not be able to eradicate HIV and AIDS on its own, it is a powerful tool in shifting the tide of an epidemic that has gripped the globe for more than three decades. Indeed, Daskalakis is confident that PrEP, in combination with existing interventions and increased education, can finally bring new HIV diagnoses below epidemic levels. But part of achieving that goal includes educating the public, elected officials, and health organizations about the impact PrEP can have. Further, he says, actually getting PrEP into the hands of those most at risk is crucial, especially since many of those communities are low-income and may not have relationships with or access to health care providers.
"I am hopeful that the political and public health stars will align and lead us to a way that covers PrEP for those who cannot otherwise not afford it," says Daskalakis. "Such assistance will be critical to propelling PrEP into the communities that most need it and may not be able to afford it. We need to get PrEP to younger men and people of diverse gender experiences who are at risk and often marginalized by the medical system."
The CDC suggests anyone who is at "substantial risk for HIV" consider taking PrEP. According to the federal agency, that includes serodiscordant couples, those in relationships that are not mutually monogamous, gay and bisexual men who have had anal sex without a condom or been diagnosed with any STI within the past six months, and heterosexual men or women who do not regularly use condoms with partners of unknown HIV status.
The CDC recommendations are notably lacking in formal guidance for transgender people -- who are statistically among the most at-risk for new HIV infections -- but Daskalakis extends the CDC's suggestion.
"[Men who have sex with men] and trans people who have condomless sex are specifically the targets for this intervention, but sexually active heterosexual men and women with risk, as well as injection or stimulant drug users, may benefit from PrEP," he explains. "It's a one-on-one decision between patient and medical provider."
As implementation of President Obama's Affordable Care Act continues to roll out nationwide, the potential exists for thousands who previously lacked insurance to gain access to plans that should include PrEP among covered preventive care.
However, the changing health care landscape can be daunting to navigate, cautions Havlir. "So one of our mandates is to make sure that those who desire to access PrEP can do so," she explains. "Programs are and need to be available to offset drug costs for those unable to afford it."
While the ACA offers insurance to a growing number of Americans, Gilead, the pharmaceutical company producing Truvada -- the only drug currently FDA-approved as PrEP -- also has a patient assistance program to help offset co-pays or minimize cost for those without insurance.
While PrEP might not be for everyone, experts who spoke with The Advocate pointed to a desirable side effect of even just considering PrEP: The more people who have a frank, honest discussion with their doctor about whether PrEP is right for them, the more people are taking a proactive role in their own health and managing the risk of contracting (and spreading) HIV or other STIs.
After starting a PrEP regimen, patients will be asked to visit their health care provider once every three months, which not only allows close monitoring of the drug's effects but also establishes a strong provider-patient relationship and supports early interventions for other infections or illnesses that might compromise the immune system.
Although PrEP is the newest and arguably one of the most exciting developments in the fight against HIV, Daskalakis is confident it won't be the last major breakthrough. In fact, additional groundbreaking treatments are on the way, and the country -- indeed, the world -- needs to be prepared to link all people at risk with access to the critical care they need.
"We need to get our infrastructure ready for the next wave of HIV prevention," says Daskalakis. "With long-acting injectable drugs coming down the pike, we need to be ethically, logistically, and unapologetically ready to support PrEP for all people at risk."