In mid January researchers in San Francisco and Boston sparked a global press circus when they reported that a virulent, multidrug-resistant form of staph bacteria (specifically, methicillin-resistant Staphylococcus aureus, or MRSA) was spreading among gay men. According to the report, Bay Area gays were 13 times more likely to be infected than area residents in general. Epidemiologist Binh An Diep, the lead researcher, summed up the findings this way: "Once this reaches the general population, it will be truly unstoppable."
The world press went wild. A London tabloid called the bug "the new HIV." An Australian paper ran the headline "Flesh-Eating Bug Spreads Among Gays." Right-wing groups piled on: "Gays May Spread Deadly Staph Infection to General Population," blared a missive from Concerned Women for America.
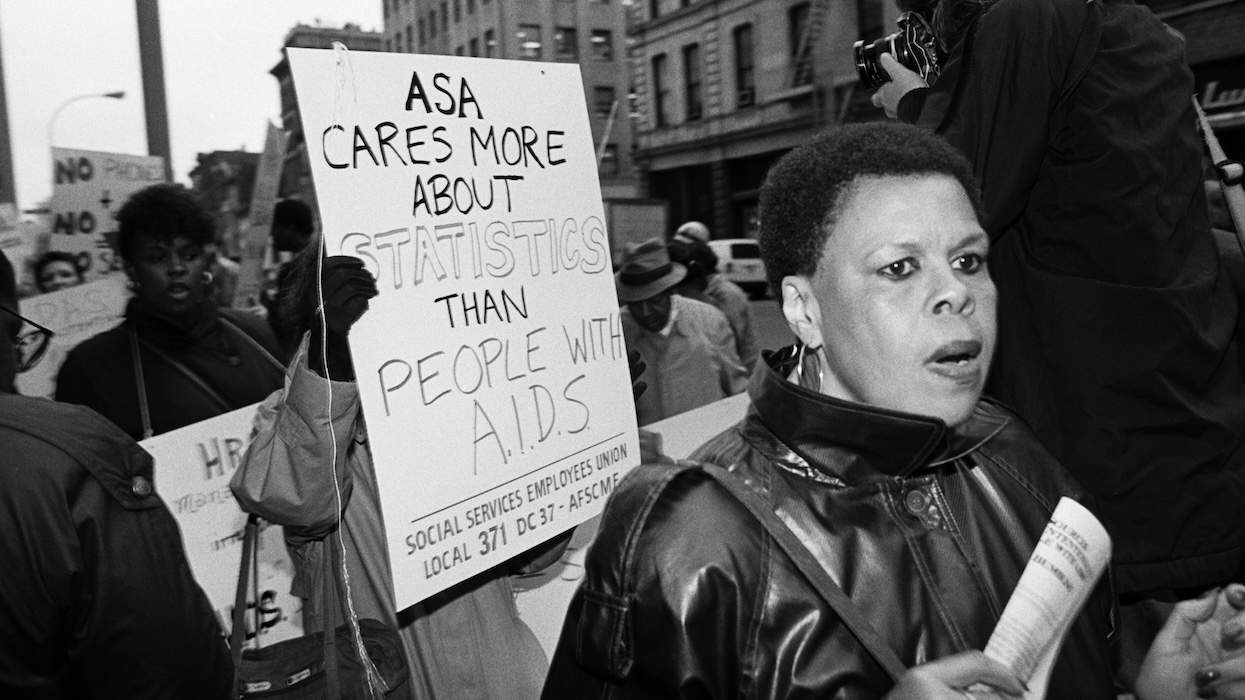
The hysteria echoed homophobic headlines from the early days of AIDS, and gay newspapers and activists quickly struck back, pointing out that MRSA was already widely reported in "the general population" and wasn't transmitted primarily through sex. "I've lost count of how many times I've seen this depressing drill about gay men, our sexuality, diseases, and researchers generating great headlines for their academic careers," wrote activist Michael Petrelis on his blog.
Within days the University of California, San Francisco, researchers apologized. In their revised press release they downplayed the role of gay men and removed the hot-button medical term "general population." Researcher Henry Chambers told The Advocate that Diep was a rookie researcher who "was not thinking about the consequences" of his word choices. "He meant that [MRSA] is more prevalent in the gay population," said Chambers, "and that it might become as prevalent in other populations as well."
Now that the kerfuffle is behind us, let's get to the facts. MRSA is not spread just through sex. It appears most commonly in hospital settings and among groups, such as football players or wrestlers, engaging in frequent skin-to-skin contact or contact with shared mats, clothes, towels, razors, and the like. It didn't originate among gays, but doctors who treat gay men in New York City, Boston, San Francisco, and Chicago say that since 2000 they have seen a marked increase in MRSA, which is resistant to penicillin antibiotics but treatable with other drugs. As for the scary "flesh-eating" moniker, in rare cases, MRSA--which begins with what usually resembles a pimple or a spider bite and blows up painfully over a few days into a pus-filled abscess--can damage skin tissue. But again, that's rare.
Ken Mayer, medical research director of Boston's LGBT-serving Fenway Community Health (which reported the Boston end of the study), says that Fenway currently sees one to two cases of MRSA a week. It's a clear increase over the past few years but not an epidemic. Tom Barrett, chief medical officer of Chicago's LGBT-focused Howard Brown Health Center, says, "Now when we see a skin infection we assume it's MRSA, because every [skin infection] we've cultured [in the lab] for several months is."
Because sex involves skin-to-skin contact, MRSA can be spread that way, which is likely why many gay men get the infection in their genital area. Of particular concern are users of drugs like crystal meth, because hours of drug-fueled sex can abrade the skin and let the infection in, especially if participants go a long time without showering. But people can also pick up infections at the gym (wear flip-flops in the showers!) and other random places. "Most of the time," says Barrett, "we haven't traced cases to sexual encounters."
Is MRSA the new HIV? Not quite. HIV is hard to transmit sexually outside of anal and vaginal intercourse, whereas MRSA can be transmitted through naked frottage alone. (Transmission through kissing or a handshake is unlikely.) Numerous studies find MRSA more common among HIV-positive gay men than their HIV-negative counterparts--in fact, the controversial report initially obscured the fact that all the cases reviewed in San Francisco and about half from Boston were in HIV-positive men--but it's unclear whether that's because the immune systems of HIV-positive men are more vulnerable or because many choose to have sex only with other HIV-positive men, thereby spreading MRSA among that group.
Yes, gay men have registered a recent rise in both MRSA and HIV (the Centers for Disease Control and Prevention tracked a 13% increase in HIV among gay men between 2001 and 2005). But "they're parallel phenomena," says Ken Mayer. "I don't think one is causing the other."
The MRSA takeaway? Pretty simple: To prevent it, wash your hands often with antibacterial soap and shower after any skin-to-skin contact or contact with possibly infected surfaces. Don't share towels, clothes, or other personal supplies with people with staph. And clean and cover any cuts or wounds.
If you have what looks like a spider bite or pimple, don't try to pop it, and if it starts leaking pus, cover it. If it grows rather than fades over a few days, get to a doctor. Now that MRSA is a known villain in the world at large, most doctors should be on the lookout for it, but just in case, suggest to your doctor that it be cultured to determine the best antibiotic.
Treatment typically involves lancing and draining the abscess, which will often do the trick, says Gal Mayer, medical director of New York City's LGBT-serving Callen-Lorde Community Health Center. But these days many doctors will assume it's MRSA and start patients right away on nonpenicillin drugs like Bactrim, clindamycin, or tetracycline. (The San Francisco-Boston study reported on a newer strain of MRSA that's resistant to two of those three meds.) In some cases hospitalization for IV treatment is required, as vividly demonstrated when Project Runway contestant Jack Mackenroth left the competition in an episode aired in December for an infection in his nose.
The bottom line is that MRSA isn't just about sex and it isn't limited to gays, but you still have to be careful. Just ask Ryan Rivera, 42, a New York City fund-raising executive who says that he and his boyfriend are both HIV-negative and monogamous. Rivera got MRSA in the summer of 2005 when he and his partner were renovating their apartment, wearing shorts and kicking up "lots of dust and dirt and germs and mold." He was hospitalized for four days and took Bactrim for a few weeks. The recent coverage "twisting it into the whole gay infection thing" infuriated him: "I've done enough research to know that it didn't start with gay guys, and it's not going to end with gay guys."














Charlie Kirk DID say stoning gay people was the 'perfect law' — and these other heinous quotes
These are some of his worst comments about LGBTQ+ people made by Charlie Kirk.