When I wanted to get gender-reassignment surgery in 1978, I had few financial options. At six feet tall, I don't think anyone particularly saw me as female, and consequentially I was unemployed.
I was lucky in three ways, though. First, my partner worked at Cleveland State University, so I knew CSU's Blue Cross/Blue Shield policy covered gender-related care. That made it a definite outlier, but with the prestigious Cleveland Clinic still doing the surgery, it was hard for the Blues to argue that gender reassignment was not legitimate care. That was my second bit of luck. The third was that the (mostly gay) men at the CSU theater department -- it was famous back then for Michael Bennett, who'd created A Chorus Line -- gave me a job as a secretary, which was how I actually got my insurance and could afford to cover the co-pays and various ancillary expenses attached to my surgery.
So I was hugely lucky. Even today, standard industry templates for group plans often include specific exceptions for transgender people. Even if they don't have caveats related to transgender care, trans people are often routinely denied coverage for the transition-related medical care they desperately need. Even when coverage is made available and the discriminatory exclusion of trans people prohibited, insurance personnel often lack any sort of training in transition-related care, and may refuse coverage or reimbursement even when a procedure is covered. In other cases, they may simply require a lot of documentation, which slows things down, or internal policies may be unclear or not well understood.
Any of these factors can shift the burden of getting reimbursed onto the patient, or simply make them postpone expensive procedures they can't afford to pay for out of pocket while waiting for a check to arrive.
So I was especially interested to learn that the trans daughter of a longtime supporter in Connecticut was about to undergo surgery and was having problems getting her gender-related care paid for. Connecticut had recently become the fifth state to require coverage for trans-related medical care, in December of 2013 (joining California, Colorado, Oregon, and Vermont). His daughter -- the subject of an earlier column of mine -- was to be the first trans person to take advantage of the new coverage. But though he was a highly placed insurance industry consultant and a recognized expert in the field, he still had to fight tooth and nail to get his daughter's transition care covered, along the way patiently educating a small army of insurance personnel who had never dealt with such a case.
Denying or delaying coverage can seem like a no-brainer for insurers; a win-win. If coverage is denied, they save money, while delaying claims keeps the money in their pockets longer. And don't forget we're dealing with a very small, marginalized minority that is routinely discriminated against. Thankfully, a federal court recently ruled that Obamacare prohibits discrimination against trans patients. While that's a great step, prejudice remains regrettably rife in the field.
"Why," my friend fumed, "doesn't anyone research the costs of not providing coverage?" After hearing this for the third time, I finally realized that he was onto something.
Working with John Hodson of True Benefit,; Dr. Marci Eads, former director of research for the Gill Foundation and currently a principal with HMACS, Dr. Dana Beyer of The Huffington Post, Gender Rights Maryland, Freedom to Work, and Anand Kalra, program administrator for the Transgender Law Center, we developed an online survey to try to address just this question. You can see it here.
The survey is the first attempt to try to capture the costs of providing, and not providing, transition-related care. The social costs of not providing care are measured a number of ways, including psychotherapy, job loss, antidepressants, eviction, etc.
We also look at other problems that arise with trying to obtain coverage -- some of which might not at first be apparent. For instance, if you live in a major city and your insurer covers your transition, you're probably in good shape. But if you live in one of the thousands of small cities and towns in rural America, chances are you can't find a trans-savvy physician in your provider network. That means you travel to a big city, maybe out of state, for someone who's out of network. You end up paying out of pocket, even though in principle your transition costs are covered.
Hopefully, we will get enough data to make some definitive statements about the impact on society when urgently needed medical care is denied. Paradoxically, we not only need trans people whose costs didn't get covered, but those who did, so we can compare them.
Looking back at Cleveland State, I was a terrible secretary, and the university rightfully let me go. But my former employer let me keep my coveted Blue Cross/Blue Shield plan. Thank God it did. With changes slowly coming to the insurance industry, hopefully many others will receive similar treatment.
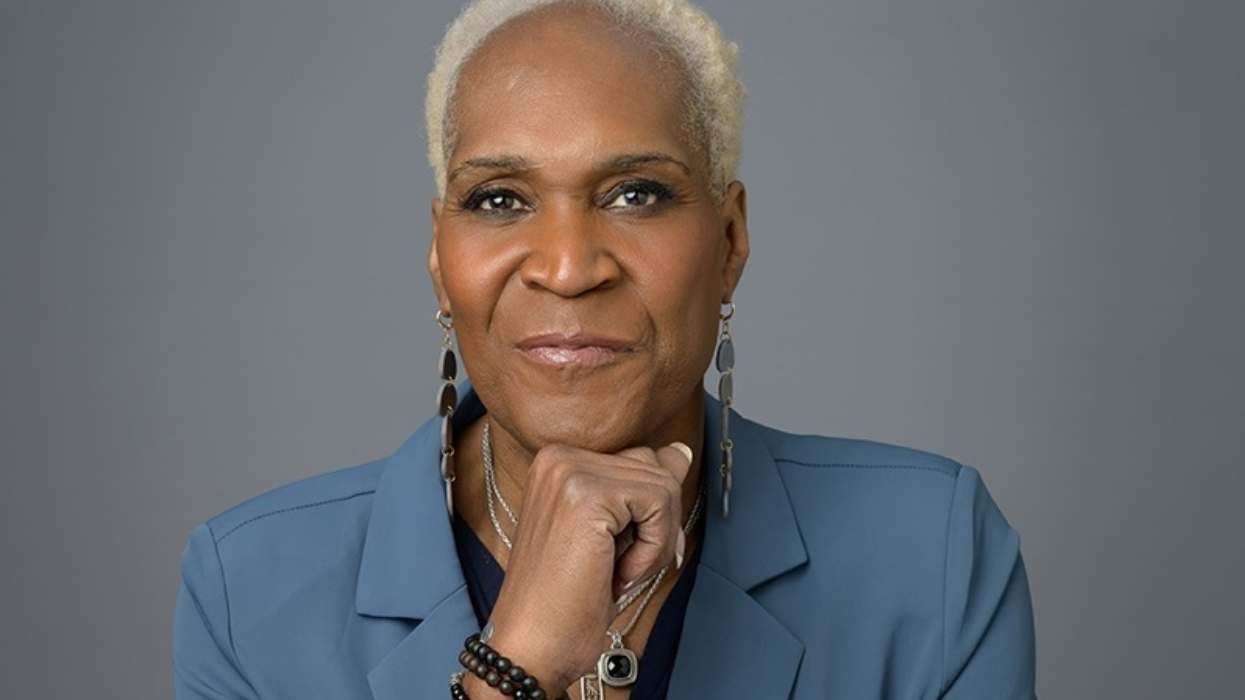
RIKI WILCHINS is the executive director of True Child, an organization that challenges rigid gender norms and inequities.

































































Charlie Kirk DID say stoning gay people was the 'perfect law' — and these other heinous quotes