The federal Department of Health and Human Services announced Thursday that it will reconsider a longstanding denial of gender-confirming surgeries for transgender people on federally subsidized healthcare.
Since 1989, both Medicare and Medicaid, the federally-run health program for low-income families and individuals, have explicitly excluded the coverage of gender confirmation surgeries for transgender individuals.
Under National Coverage Determination 140.3, the programs have been exempted from covering these surgeries, though the data cited in the government's justification is based on a 1981 National Center for Health Care Technology report. "Because of the lack of well controlled, long term studies of the safety and effectiveness of the surgical procedures and attendant therapies for transsexuals, the treatment is considered experimental," reads the report in its explanation for why such procedures are not covered by insurance. "Moreover, there is a high rate of serious complications for these surgical procedures. For these reasons, transsexual surgery is not covered."
A lot has changed since 1981, however. The American Medical Association and American Psychological Association have since issued statements in support of gender-confirmation surgeries as a medical necessity and acceptable treatment for those suffering from gender dysphoria.
In a ruling released December 2, the Department of Health and Human Services Departmental Appeals Board declared that the current National Coverage Determination record "is not complete and adequate to support the validity" of the determination excluding coverage for gender-confirming surgeries. The board determined that the 1981 report, which reviewed medical and scientific sources published between 1966 and 1980, is no longer "reasonable in light of subsequent developments."
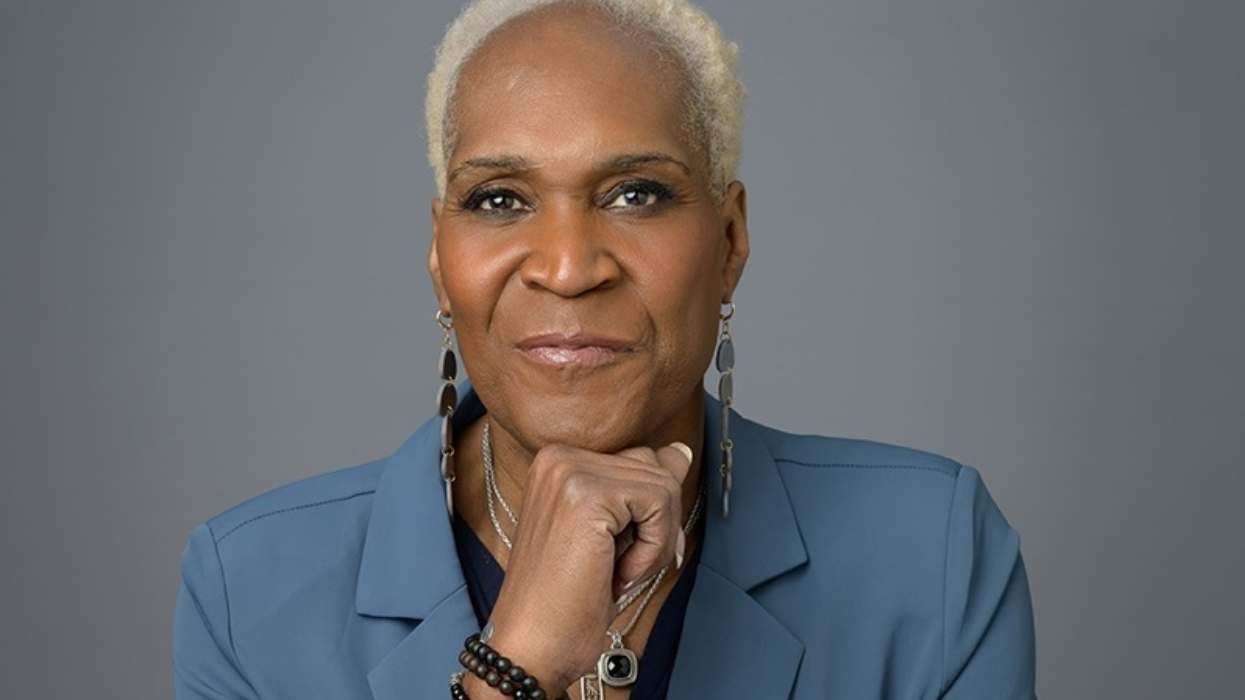
The 10-page ruling states that the aggrieved parties, which included the National Center for Lesbian Rights, the American Civil Liberties Union, Gay and Lesbian Advocates and Defenders, and civil rights attorney Mary Lou Boelcke, believe that the bases for the National Coverage Determination are flawed. "These bases for the NCD neither 'reflect nor are supportable by the current state of medical science,' and the NCD 'is not reasonable in light of the current state of scientific and clinical evidences and current medical standards of care,'" reads the decision.
The ruling goes on to cite the fact that "dozens of new studies have been conducted that... confirm that sex reassignment surgery is a safe and extremely effective treatment for individuals with severe gender dysphoria; advancements in surgical techniques have dramatically reduced the risk of complications from sex reassignment surgery;" and also that "a robust medical consensus has developed among mainstream medical organizations which endorse the treatment standards established by the World Professional Association for Transgender Health," which deems such clinical treatment medically necessary.
The Centers for Medicare and Medicare Services did not refute any of the claims made in support of gender-confirming surgery, which means the Department will now proceed to the discovery stage of the appeals process, determining whether or not the current ban on Medicaid coverage for gender confirmation surgeries will stand. It is not known when this process will be complete.


































































Charlie Kirk DID say stoning gay people was the 'perfect law' — and these other heinous quotes